-
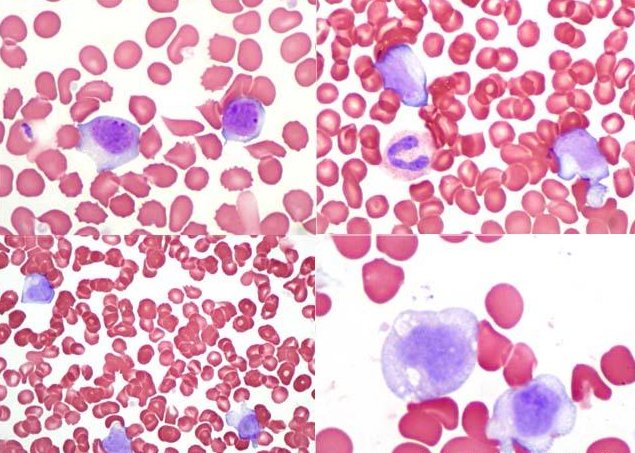
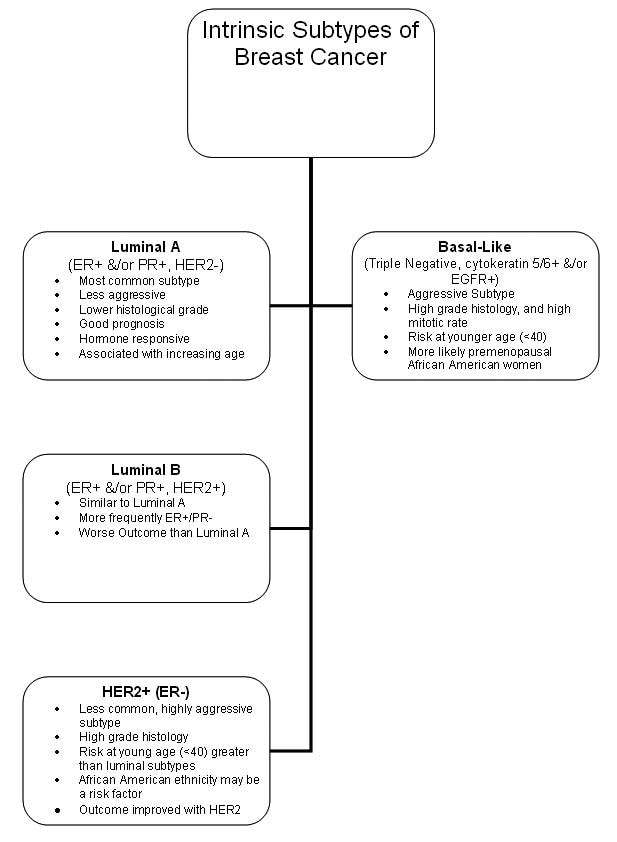 Sottotipi intrinseci di cancro al seno.
Sottotipi intrinseci di cancro al seno. -
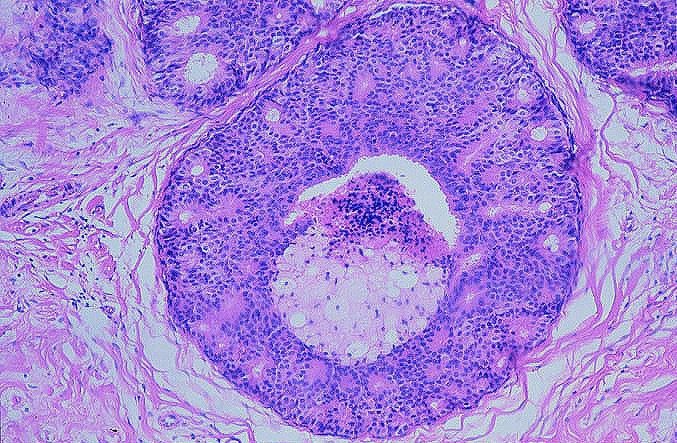 Cancro al seno. Carcinoma intraduttale, tipo comedo. Dotto disteso con membrana basale intatta e necrosi tumorale centrale
Cancro al seno. Carcinoma intraduttale, tipo comedo. Dotto disteso con membrana basale intatta e necrosi tumorale centrale -

Un carcinoma invasivo infiltrante è un tumore le cui cellule hanno acquisito la potenzialità invasiva e la possibilità di diffusione a distanza (metastasi).
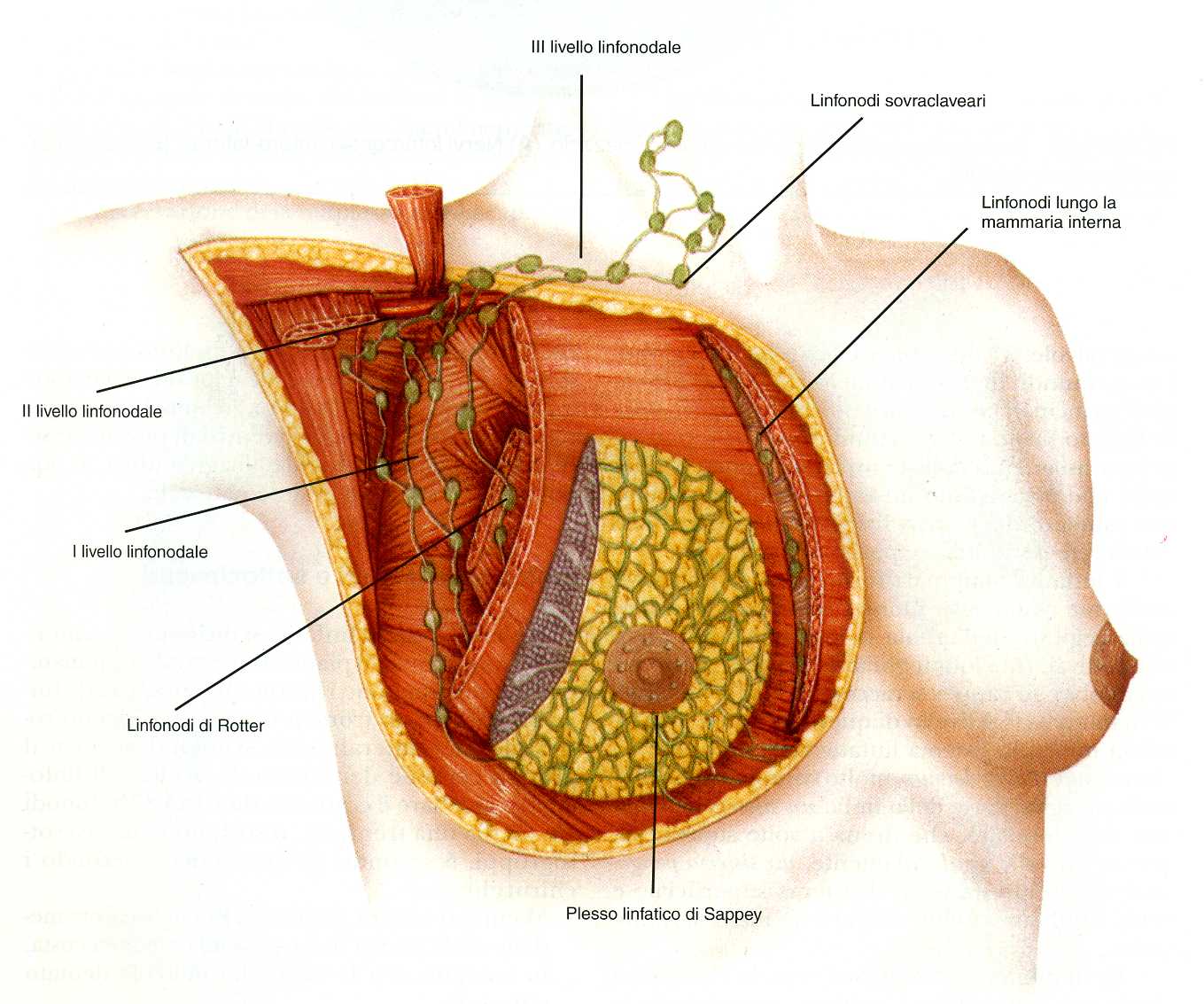
I carcinomi invasivi della mammella si diffondono per via linfatica dando metastasi in primo luogo ai linfonodi ascellari. Lo stato linfonodale ascellare è il principale fattore prognostico.
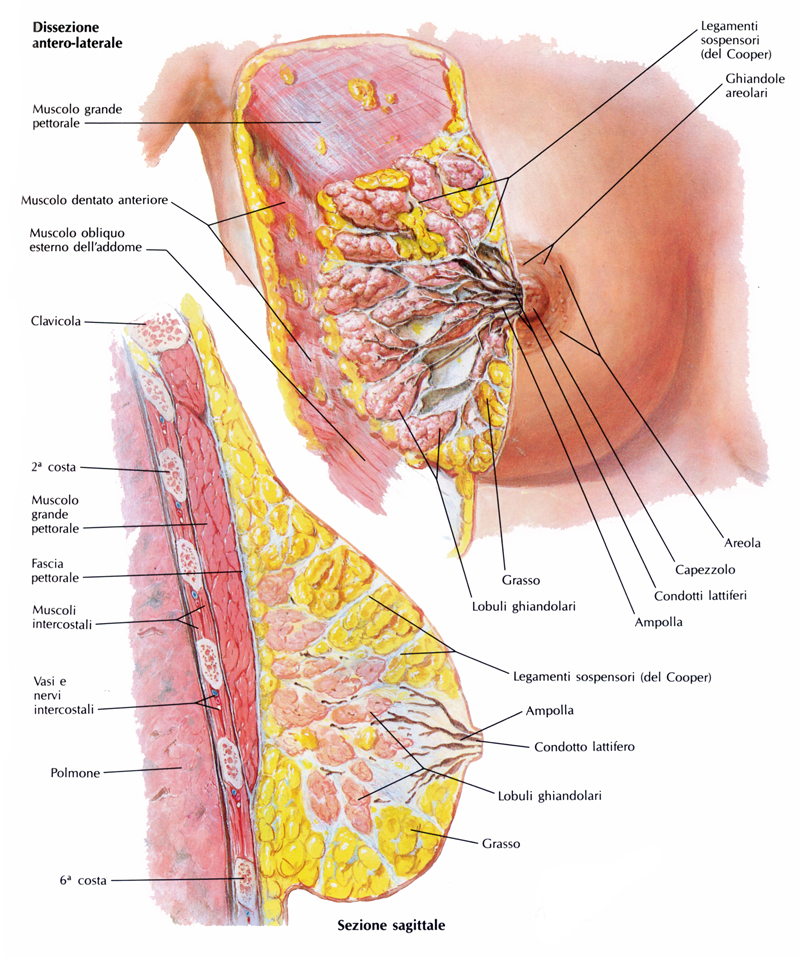
Il carcinoma della mammella origina dalle cellule epiteliali della ghiandola e può dar luogo a diversi tipi istologici.
Istotipi e relativa frequenza
– carcinoma duttale infiltrante 75 %
– carcinoma lobulare infiltrante 15 %
– carcinoma midollare 5 %
– carcinoma mucinoso 2 %
– carcinoma tubulare 1 %
– carcinoma infiammatorio < 1 %
– malattia di Paget < 1 %
– cistosarcoma filloide < 1 %
I più diffusi sono il carcinoma duttale ed il lobulare. Il carcinoma in assoluto più frequente è il duttale infiltrante caratterizzato da abbondante stroma che gli conferisce un aspetto duro. E’ denominato duttale pur originando dall’unità terminale duttulo-lobulare.
La metà dei casi insorge nel quadrante supero-esterno della mammella ed il 20% nel settore centrale.
La maggiore diffusione del tumore nel quadrante supero-esterno è legata al fatto che in questo settore è presente la parte prevalente di tessuto ghiandolare.
Il carcinoma lobulare della mammella pur essendo a prognosi migliore rispetto al duttale è il tumore di più difficile interpretazione diagnostica perché spesso non è irregolare ed alla palpazione non è consistente. Può essere multicentrico e multifocale e nel 20% dei casi bilaterale.
Il carcinoma mucinoso ed il carcinoma tubulare sono associati a bassi tassi di invasione linfonodale ed a metastasi a distanza.
Il carcinoma midollare è caratterizzato da un alto indice nucleare, infiltrazione linfocitaria e da un quadro di crescita sinciziale. E’ ritenuto a basso potenziale metastatico.
La mastite carcinomatosa è una varietà aggressiva di carcinoma invasivo che infiltra i vasi linfatici della cute e conferisce alla pelle della mammella un aspetto detto “a buccia d’arancia” con una reazione infiammatoria della parte interessata che diventa rossa, tumefatta e dolente. I segni radiologici della mastite carcinomatosa non sono caratteristici e non si differenziano da un processo flogistico.

 Con il termine Malattia di Paget si indica un carcinoma in situ o invasivo in cui le cellule tumorali si diffondono nella cute in direzione del capezzolo e della areola. Nel 40% dei casi la Malattia di Paget è associata ad un tumore invasivo.
Con il termine Malattia di Paget si indica un carcinoma in situ o invasivo in cui le cellule tumorali si diffondono nella cute in direzione del capezzolo e della areola. Nel 40% dei casi la Malattia di Paget è associata ad un tumore invasivo.
Il cistosarcoma filloide è la varietà maligna del tumore filloide e comporta capacità metastatica soprattutto per via ematica.
L’incidenza del carcinoma bilaterale della mammella risulta poco superiore al 3% del totale dei cancri della mammella.
Esistono delle situazioni cliniche particolari come il carcinoma mammario della mammella maschile (1% dei tumori mammari) ed il carcinoma mammario in gravidanza i cui istotipi non variano ma la cui specificità è nel trattamento.
Breast Cancer Staging
Lo stadio di un cancro al seno descrive le sue dimensioni e la sua diffusione. Il sistema di stadiazione va dalla fase 0 alla fase IV in base alle dimensioni del tumore, linfonodi coinvolti, e metastasi a distanza.
T indica le dimensioni del tumore. La lettera T è seguita da un numero da 0 a 4, che descrive la dimensione del tumore e se è diffuso sulla cute o sulla parete toracica . Numeri T elevati indicano un tumore più grande e / o più ampia diffusione ai tessuti circostanti il seno.
- TX: Il tumore non può essere valutato.
- T0: Nessuna evidenza di un tumore è presente.
- Tis: il tumore può essere LCIS, DCIS, o malattia di Paget.
- T1: il tumore è di 2 cm o più piccolo in diametro.
- T2: Il tumore è di 2-5 cm di diametro.
- T3: Il tumore è più di 5 cm di diametro.
- T4: Il tumore è qualsiasi dimensione, e ha infiltrato la parete toracica e diffuso ai pettorali (petto) linfonodi.
N indica i linfonodi palpabili. La lettera N è seguita da un numero da 0 a 3, che indica se il tumore si è diffuso ai linfonodi vicino al seno e, in caso affermativo, se i linfonodi interessati sono fissati ad altre strutture sotto il braccio.
- NX: I linfonodi non possono essere valutati (ad esempio, i linfonodi sono stati precedentemente rimossi).
- N0: il tumore non è diffuso ai linfonodi.
- N1: il tumore è diffuso ai linfonodi ascellari omolaterali mobili (ascellare linfonodi sullo stesso lato del tumore al seno).
- N2: il tumore ha invaso i linfonodi omolaterali (sullo stesso lato del corpo come il cancro al seno), fissati tra loro o ad altre strutture sotto il braccio.
- N3: il tumore si è diffuso ai linfonodi mammari omolaterali o ai nodi omolaterali linfonodi sovraclaveari (sullo stesso lato del corpo come il cancro al seno).
M indica metastasi. La lettera M è seguita da un 0 o 1, e indica se il cancro ha metastatizzato in organi distanti (ad esempio, i polmoni o ossa) o ai linfonodi non adiacenti al seno, come quelli sopra la clavicola.
- MX: metastasi non può essere valutata
- M0: Non metastasi a distanza ad altri organi è presente
- M1: si è verificato metastasi a distanza ad altri organi
Breast Cancer Histology
Updated: May 24, 2018
- Author: Peter Abdelmessieh, DO, MSc; Chief Editor: Marie Catherine Lee, MD, FACS ..
Ductal Carcinoma In Situ
Ductal carcinoma in situ (DCIS) is noninvasive breast cancer that is limited to the inside of the ducts of the breast. Increased use of screening mammography has resulted in a dramatic increase in the detection of ductal carcinoma in situ (DCIS). Approximately 64,000 cases of DCIS are diagnosed annually in the United States. Ninety percent of DCIS cases are identified on mammography as suspicious calcifications, with a linear, clustered, segmental, focal, or mixed distribution.
DCIS is categorized as low grade (grade I), intermediate grade (grade II), or high grade (grade III). Grading is based on characteristics of nuclei. Designation as low- and intermediate-grade DCIS implies that the cancer cells are growing at a relatively slow rate. Women with low-grade DCIS are at higher risk of developing invasive breast cancer than women without DCIS, but are less likely to have a recurrence of the breast carcinoma or to develop new cancers than women with higher-grade DCIS.
Low-grade DCIS cells appear very much like normal breast cells or atypical ductal hyperplasia cells. Grade II DCIS cells look less like unaffected cells and grow faster than normal. High-grade DCIS cells are growing rapidly; grade III DCIS has the highest risk of progressing to invasive cancer within the first 5 years after diagnosis.
Review of DCIS by a pathologist can identify prognostic features. Pathologists look at the following four distinct histologic features:
- Tumor size
- Necrosis presence
- Nuclear grade
- Width of surgical margin
The Van Nuys Prognostic Index [1] is an attempt to objectively determine the aggressiveness of DCIS and the probability that local recurrence will occur after breast-conserving therapy (surgery). See Table 1, below.
Table 1 The Van Nuys Prognostic Index (VNPI) Scoring System (Open Table in a new window)
| Score* | 1 | 2 | 3 |
| Size | < 15 mm | 16-40 mm | >41 mm |
| Margins | >10 mm | 1-9 mm | < 1 mm |
| Pathologic
Classification |
Non–high grade without necrosis (nuclear grade 1 and 2) | Non–high grade with necrosis (nuclear grade 1 and 2) | High grade with or without necrosis (nuclear grade 3) |
| *Scores for tumor size, surgical margin, and pathologic classification are added to produce a total VNPI score of 3 to 9, with increasing scores representing a progressively worse prognosis. | |||
DCIS is divided into comedo (ie, cribriform, micropapillary, solid) and noncomedo subtypes.This division provides additional prognostic information on the likelihood of progression or local recurrence (see the images below). Less common subtypes of DCIS are as follows:
- “Clinging” carcinoma in situ [9]
- Intraductal signet ring carcinoma
- Cystic hypersecretory duct carcinoma
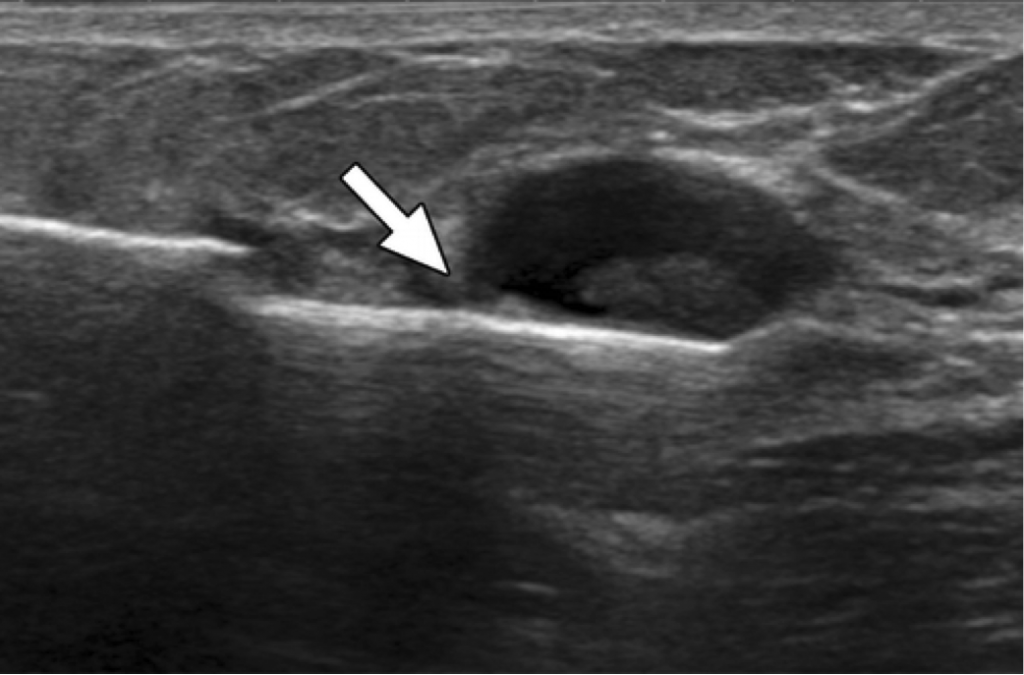
Breast cancer. Intraductal carcinoma, comedo type. Distended duct with intact basement membrane and central tumor necrosis.
View Media Gallery
Breast cancer. Intraductal carcinoma, noncomedo type. Distended duct with intact basement membrane, micropapillary, and early cribriform growth pattern
View Media Gallery
Lobular Carcinoma In Situ
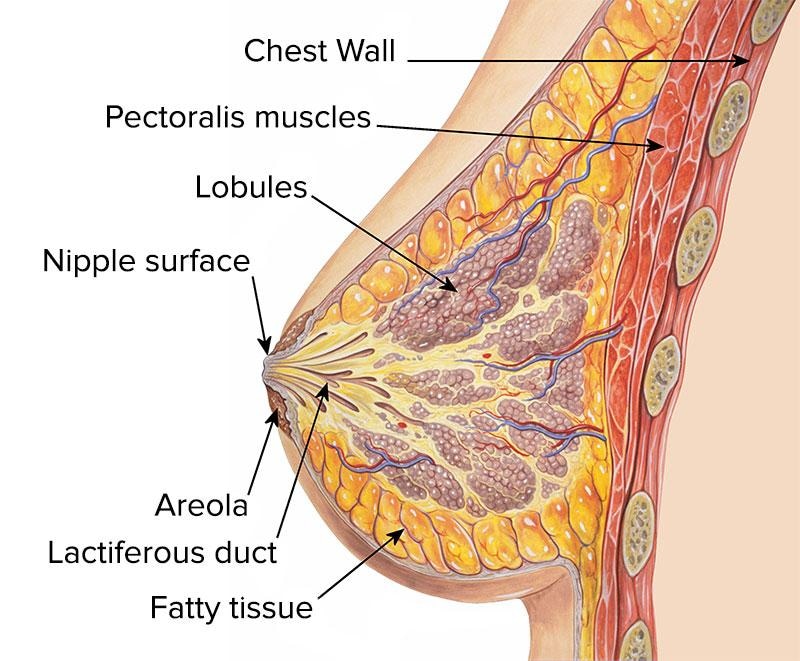
Lobular carcinoma in situ (LCIS), which is not considered a malignancy, arises from the lobule at the terminal end of the duct and shows a rather diffuse distribution throughout the breast, which explains its presentation as a nonpalpable mass in most cases (see the images below). Over the past 25 years, LCIS incidence has doubled and is currently 2.8 per 100,000 women. The peak incidence is in women aged 40-50 years.
Breast cancer. Lobular carcinoma in situ. Enlargement and expansion of lobule with monotonous population of neoplastic cells.
View Media Gallery
Breast cancer. Lobular carcinoma in situ at high power view showing orderly cells uniformly arranged with very few or no mitoses.
View Media Gallery
A study by Tran-Thanh et al found that the prolactin receptor gene is a potentially important target in the pathogenesis and progression of lobular neoplasia. Because this gene was found to be potentially less important in ductal carcinomas, the conclusion is that lobular and ductal carcinomas may evolve along separate pathways [2]
Invasive Carcinoma
Invasive ductal carcinoma
Invasive ductal carcinoma is the most commonly diagnosed breast cancer and has a tendency to metastasize via lymphatics. This lesion, which accounts for 75% of breast cancers, has no specific histologic characteristics other than invasion through the basement membrane of a breast duct, as seen in the image below. DCIS is a frequently associated finding on pathologic examination.
Breast cancer. Infiltrating ductal carcinoma. Low-grade carcinoma with well-developed glands invading the fibrous stroma.
The National Comprehensive Cancer Network [3] recommends using the Nottingham Criteria [4] in grading invasive carcinoma of the breast. [4] Separate scores are given for gland (acinus) formation, nuclear atypica/pleomorphism, and mitosis counts.
Gland (acinus) formation is scored as follows:
- Score 1: >75% of the whole carcinoma forms acini
- Score 2: 10-75% of the whole carcinoma forms acini
- Score 3: < 10% of the whole carcinoma forms acini
Nuclear atypia/pleomorphism is scored as follows:
- Score 1: Nuclei only slightly larger than benign breast epithelium (< 1.5 × normal area); minor variation in size, shape, and chromatin pattern
- Score 2: Nuclei distinctly enlarged (1.5–2 × normal area), often vesicular, nucleoli visible; may be distinctly variable in size and shape but not always
- Score 3: Markedly enlarged vesicular nuclei (>2 × normal area), nucleoli often prominent; generally marked variation in size and shape but atypia not necessarily extreme
Mitosis counts, which involve a pathologist counting cells with definite mitosis in 10 consecutive fields, result in a score of 1-3.
Final grading results from the addition of all the above, with a total score between the range of 3-9. Scores and grades are as follows:
- Total score 3-5 = grade 1
- Total score 6 or 7 = grade 2
- Total score 8 or 9 = grade 3
Invasive lobular carcinoma
Invasive lobular carcinoma has a much lower incidence than infiltrating ductal carcinoma, constituting less than 15% of cases of invasive breast cancer. It is characterized histologically by the “Indian file” arrangement of small tumor cells.
Staining for E-cadherin can add in distinguishing lobular carcinoma from invasive ductal carcinoma. Studies have illustrated a link between cadherin (CDH1) gene and invasive lobular breast cancers, with approximately 50 % of this subtype of breast cancer containing E-cadherin mutations. However, like ductal carcinoma, infiltrating lobular carcinoma typically metastasizes to axillary lymph nodes first. However, it also has a tendency to be more multifocal. Despite that, the prognosis is comparable to that of ductal carcinoma. [1]
Medullary Carcinoma
Medullary carcinomas appear commonly in a younger patient population, and are more frequent in women who have BRCA1 gene mutations. These tumors have a more favorable prognosis that infiltrating ductal carcinoma. Most patients present with a bulky palpable mass with axillary lymphadenopathy. Diagnosis of this type of breast cancer depends on the following histologic triad:
- Sheets of anaplastic tumor cells with scant stroma
- Moderate or marked stromal lymphoid infiltrate
- Histologic circumscription or a pushing border
Mucinous Carcinoma
Mucinous (colloid) carcinoma is another rare histologic type, seen in fewer than 5% of invasive breast cancer cases. It usually presents during the seventh decade of life as a palpable mass or appears mammographically as a poorly defined tumor with rare calcifications, and tends to be well circumscribed
Mucin production is the histologic hallmark. Two main forms occur, type A and B, with AB lesions possessing features of both. Type A mucinous carcinoma represents the classic variety with larger quantities of extracellular mucin (see the image below), whereas type B is a distinct variant with endocrine differentiation, with histology showing more granular cytoplasm then type A carcinomas. [5]
Breast cancer. Colloid (mucinous) carcinoma. Nests of tumor cells in pool of extracellular mucin
Tubular carcinoma of the breast is an uncommon histologic type constituting 1-2% of all breast cancers. Characteristic features of this type include a single layer of epithelial cells with low-grade nuclei and apical cytoplasmic snoutings arranged in well-formed tubules and glands.
Tubular components constitute more than 90% of pure tubular carcinomas and at least 75% of mixed tubular carcinomas. This type of breast cancer has a low incidence of lymph node involvement and a very high overall survival rate. Because of its favorable prognosis, patients are often treated with only breast-conserving surgery and local radiation therapy.
Papillary Carcinoma
Papillary carcinoma of the breast encompasses a spectrum of histologic subtypes. There are two common types: cystic (noninvasive form) and micropapillary ductal carcinoma (invasive form). Papillary breast cancer is usually seen in women older than 60 years and accounts for approximately 1-2% of all breast cancers. Papillary carcinomas are centrally located in the breast and can present as bloody nipple discharge. They are strongly estrogen receptor (ER) positive and progesterone receptor (PR) positive.
Cystic papillary carcinoma has a low mitotic activity, which results in a more indolent course and a good prognosis. However, invasive micropapillary ductal carcinoma has a more aggressive phenotype, even though approximately 70% of cases are ER positive. A retrospective review of 1,400 cases of invasive carcinoma identified 83 cases (6%) with at least one component of invasive micropapillary ductal carcinoma.
Additionally, lymph node metastasis is seen frequently in this subtype (70-90% incidence), and the number of lymph nodes involved appears to correlate with survival.
Metaplastic Breast Cancer
Metaplastic breast cancer (MBC) accounts for less than 1% of breast cancer cases, tends to occur in older women (average age of onset in the sixth decade), and has a higher incidence in blacks. It is characterized by a combination of adenocarcinoma plus mesenchymal and epithelial components.
MBC encompasses a wide variety of histologic patterns, including the following:
- Spindle-cell carcinoma
- Carcinosarcoma
- Squamous cell carcinoma of ductal origin
- Adenosquamous carcinoma
- Carcinoma with pseudosarcomatous metaplasia
- Matrix-producing carcinoma
This diverse group of malignancies is identified as a single entity based on a similarity in clinical behavior. Compared with infiltrating ductal carcinoma, MBC tumors have the following characteristics:
- Larger size
- More rapid growth
- Commonly node-negative
- Typically ER negative, PR negative, and HER2negative
Phyllodes Tumor
Phyllodes tumors rare tumors of the breast, accounting for less than 1% of breast tumors. The name “phyllodes,” which is taken from the Greek language and means “leaflike,” refers to that fact that the tumor cells grow in a leaflike pattern. These tumors may be considered benign, borderline, or malignant depending on the following histologic features:
- Stromal cellularity
- Infiltration at the tumor’s edge
- Mitotic activity
Malignant phyllodes tumours behave like sarcomas and are known to develop hematogenous metastases. Occurrence is most common in premenopausal women age 40 and 50. The hematogenous spread of this subtype of breast cancer makes wide local excisional biopsy paramount, as chemotherapy or radiation are not effective in recurrent or metastatic disease.
Mammary Paget Disease
Mammary Paget disease (MPD) is relatively rare, constituting 1-4% of all breast cancers. Peak incidence is seen in the sixth decade of life (mean age, 57 years).
This adenocarcinoma is localized within the epidermis of the nipple-areola complex and is composed of the histologic hallmark Paget cells within the basement membrane. Paget cells are large, pale epithelial cells with hyperchromatic, atypical nuclei, dispersed between the keratinocytes singly or as a cluster of cells.
Lesions are predominantly unilateral, developing insidiously as a scaly, fissured, oozing, or erythematous nipple-areola complex. Retraction or ulceration of the nipple is often noted, along with symptoms of itching, tingling, burning, or pain.
Inflammatory Breast Cancer
Inflammatory breast cancer (IBC) is a highly aggressive locally advanced breast cancer. It is rare, comprising only 1 to 5% of invasive breast cancers. Due to its aggressive nature, patients often have lymph node involvement and distant metastatic disease at the time of presentation. IBC is characterized by diffuse erythema and edema (peau d’orange) involving a third or more of the skin of the breast (see the image below).
Inflammatory breast cancer illustrating the classical peau d’orange of involved skin. Courtesy of Dr Giorgio M Baratelli, Radiopaedia.org, rID 43353.
View Media Gallery
The classic histologic finding in inflammatory breast cancer is dermal lymphatic invasion by tumor cells on skin punch biopsy of the affected breast. These malignant cells form tumor emboli (see the image below), which are responsible for both the local signs and clinically inflammatory symptoms.
Histologic section of an inflammatory breast cancer specimen. Courtesy of Sofia D Merajver, MD, PhD.
View Media Gallery